A&E decision s `regrettable but correct' says doctors' chairman
Dr. David Farren tells Julie-Ann Spence there was no alternative if patient safety was to be maintained at Lagan Valley
 THE Chairman of the British Medical Association's Junior Doctors
Committee in Northern Ireland, Dr. David Farren, has said there was no
alternative but to close the Lagan Valley Hospital's Accident and
Emergency Department at night. He said that whilst the move is
regrettable, it is essential for the safety of patients.
THE Chairman of the British Medical Association's Junior Doctors
Committee in Northern Ireland, Dr. David Farren, has said there was no
alternative but to close the Lagan Valley Hospital's Accident and
Emergency Department at night. He said that whilst the move is
regrettable, it is essential for the safety of patients.
Dr. Farren, who himself trained at the Lagan Valley, said he has been trying to raise awareness of the shortage of junior doctors for the last two years and that the problem is not confined to Northern Ireland, but is affecting the whole of the UK.
Changes to immigration laws and doctors working hours have resulted in vacancies in a number of specialties, including obstetrics and emergency medicine, but Dr. Farren insists work is being done to fill the gaps.
"There is a UK wide shortage of junior doctors," explained Dr. Farren. "This has been the case since 2007 and it has got worse year on year. The gaps are at a specific level, at what used to be the Registrar grade. It is not just a case of bringing people in at the bottom level. The vacancies are for senior junior doctors and cannot be filled by graduates straight out of medical school.
"I have been the Chairman of the Junior Doctors' Committee for two years and this has been the story over those two years. I have been warning that services would have to close.
Why the crisis has arrived now
ACCORDING to Dr Farren there are three main causes of the current shortage of junior doctors.
1: Inadequate Workforce Planning several years ago. That assesses how many doctors will be needed in hospitals in 10 to 15 years time. However, when the current workforce was planned, two other factors, which had a major impact on the number of doctors needed in hospitals, had not been foreseen - a new EU working time directive and new immigration laws.
2: The European Working Time Directive reduced the hours which doctors are allowed to work from 100 a week to 48. That has meant that many more doctors are needed in hospitals. There has been a steady reduction in doctors' hours over the past ten years, firstly to 65 hours, then 58, 56, 52 and finally 48 hours. However, the last workforce planning exercise only accounted for a reduction to 56 hours, meaning at least two additional doctors are needed on the rota each week.
3: New Immigration laws. The new laws made it very difficult, if not impossible, for doctors from the sub-Indian continent to secure work in the UK. It has previously been recorded that some 25% of doctors in Northern Ireland were from outside the EU, meaning that Northern Ireland was particularly hard hit by the new laws.
Dr. Farren admits that none of these factors are easily resolved but insisted that increased numbers of doctors currently training, as well as trawls of doctors from Eastern Europe, would mean that gaps in the service would be filled in coming years.
In fact, he expressed serious concern that it may actually lead to jobs being oversubscribed in years to come, resulting in the very real risk of medical students not being able to secure a post after graduation.
"The vast majority of things that could have been done have been done. The Medical and Dental Training Agency went on a recruitment drive to the Indian subcontinent but unfortunately that didn't yield a great slumber of doctors, mainly because of immigration control and because they couldn't secure visas.
"They also put tenders out to bring doctors from mainland Europe and I am told some have been recruited from Eastern Europe.
"There is not a single person to blame for the current situation," he continued. "Workforce planning in the past has not been as good as it should have been. There was a report in 2006 that looked at workforce planning which stated the number of doctors needed but what they didn't foresee was the European Working Time Directive because there was an exception for doctors. Over the past ten years they have been trying to increase the number of doctors but the problem worsened with the change to immigration rules.
"At the minute the decision to close the A&E at Lagan Valley at night is the correct one, we don't have enough staff. It is a difficult decision but the right one. Patient safety cannot be compromised.
"This shortage of doctors is not just in Northern Ireland and hospitals in England, Scotland and Wales are having to do the same thing.
"The BMA has been saying for a number of years that we need a reconfiguration of services in a planned way so that services are not lost and departments are not closed so quickly.
IIt is regrettable that Lagan Valley A&E cannot stay open 24/7 but we
are glad the decision has been made. It is our responsibility to inform
people properly and let people know the true reasons. We have limped
along and the rota gaps have increased. Bringing m doctors at the bottom
end, which is good in the long term, doesn't effect things in the short
term. These gaps will be there for another two years. The recent
graduates from Queens will have to finish their pre-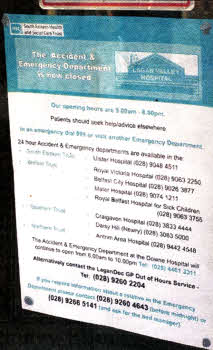 registration and in
two years time they will be applying for registrar level jobs and they
will start to make these gaps less of a problem.
registration and in
two years time they will be applying for registrar level jobs and they
will start to make these gaps less of a problem.
"Medical schools have increased student numbers so we have five years worth of medical students to fill the gaps but people starting in September face the real chance of coming out and not having a job to go to. It is worrying that we are training doctors who will end up travelling outside the UK to work, or even worse, letting their degree go to waste.
"Having worked in the Lagan Valley, it is a hospital in which I thought I got the best training of my career and it is regrettable that this has happened but it is not helpful for fingers to be pointed at junior doctors. Junior doctors have worked very hard to ensure this doesn't happen. Rather than slinging mud we should be working together to prevent this happening again," he concluded.
Lots of graduates - so why can't they fill the vacant posts at LVH
 TRAINING
to be a doctor is a long process and whilst hundreds of students have
just graduated from Queen's University Medical School, they are not yet
qualified enough to apply for the vacancies at the Lagan Valley
Hospital's A&E department.
TRAINING
to be a doctor is a long process and whilst hundreds of students have
just graduated from Queen's University Medical School, they are not yet
qualified enough to apply for the vacancies at the Lagan Valley
Hospital's A&E department.
Dr. Farren explained the training a doctor must go through and why graduates cannot be used to fill the vacancies in local hospitals.
"When a medical student qualifies they apply for a foundation programme (junior house officer) for two years. For the first year they have to work in hospitals under senior supervision. It is purely hospital based and they will be in general medical and general surgical wards.
"In the second year doctors start to rotate depending on the quality of their application and interview, they choose what rotation to go into. A list of rotations is produced and doctors choose one. When you choose your rotation you have to work where the staffing need exists. There are currently no gaps in staff for years one and two of the foundation programme.
"Once the foundation programme is done, doctors decide what they want to become and apply for a job, for example a GE consultant, specialist doctor, and start training towards an end point. If you want to work in A&E then you apply for a specialty in emergency medicine.
"Generally speaking with rotational training, when you accept the job it is on the understanding that you will be cycled around hospitals in Northern Ireland. If you are doing A&E you will go to all hospitals unless there are exceptional circumstances.
"Doctors who have recently graduated will have to finish their pre-registration year and in two years time they will be applying for Registrar level jobs."
julieann.spence@ulsterstar.co.uk/
Ulster Star
12/8/2011

